Common themes in geriatric emergency general surgery: a narrative review
Accepted: May 21, 2024
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
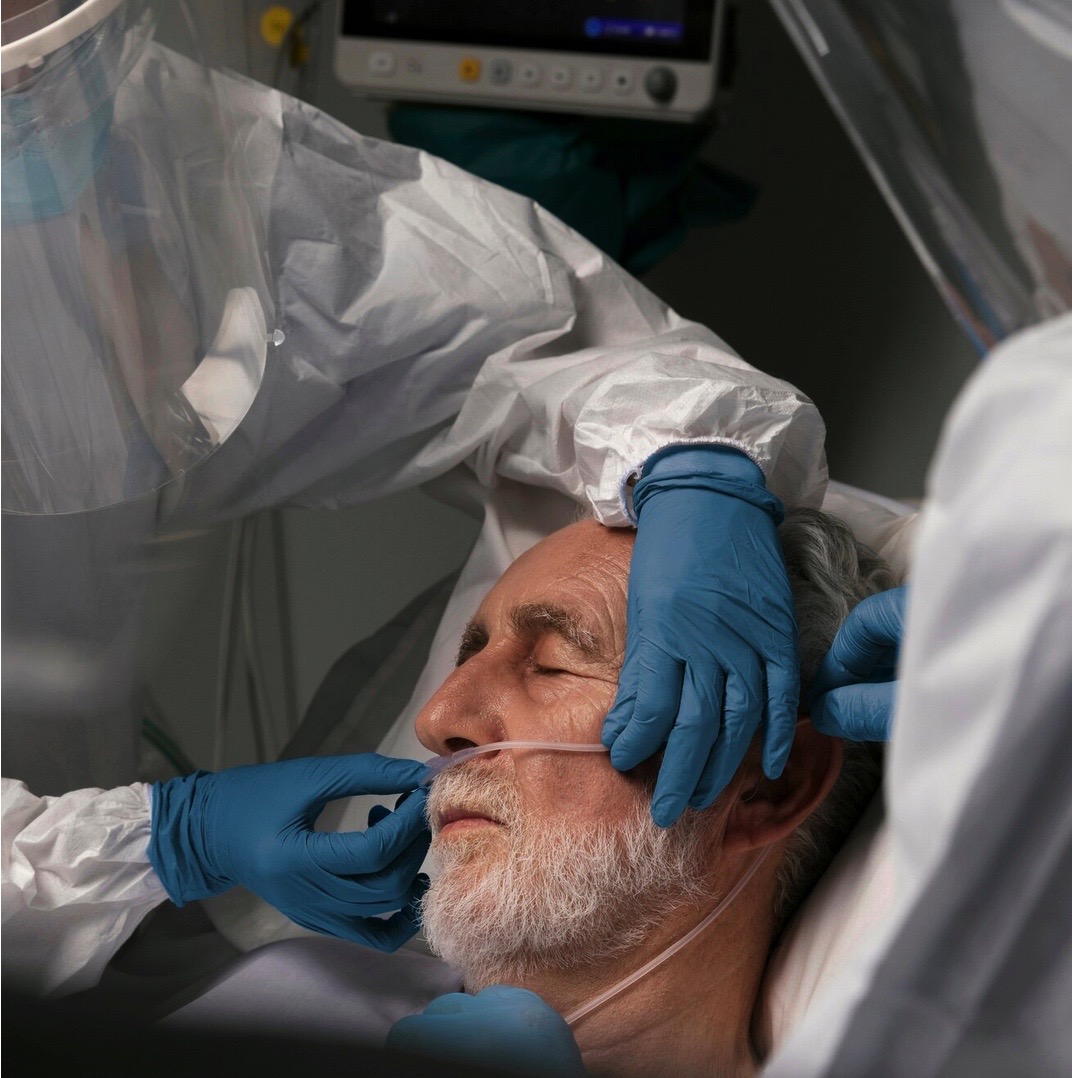
Population aging is a growing phenomenon. The geriatric patient is defined by physical, psychological, and social characteristics associated with aging that make him or her more fragile and susceptible. An older patient is usually fragile: frailty has a linear, if not unambiguous, relationship with age. With this background, the concept of futility emerges in emergency surgery, which refers to having a goal but being almost certain of failure in achieving it. A narrative review of the literature was carried out using PubMed, Google Scholar, and Cochrane to identify pertinent publications. Inclusion criteria included: i) an emergency setting in geriatric general surgery, ii) frailty in emergency surgery, and iii) futility in emergency surgery. The study identified valid assessment scores for older and frail patients, as well as imaging tools that may aid in the evaluation of frailty, demonstrating the potential futility of surgical treatment. The review addressed the most common acute surgical situations that affect geriatric patients. Older patients are more fragile and vulnerable than the general population, even though geriatric age does not always correlate with frailty. Several fragility scores have been developed to perform an accurate preoperative assessment of the urgent elderly surgical patient, to estimate treatment futility and perioperative risk, and to guide the surgeon to the most appropriate therapeutic or palliative action.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
Similar Articles
- Raffaele Bova, Giulia Griggio, Carlo Vallicelli, Luca Ansaloni, Massimo Sartelli, Federico Coccolini, Francesca Bravi, Vanni Agnoletti, Fausto Catena, APEROLD study: acute peritonitis in the oldest nonagenarian patients with acute abdomen. Which is the fate? , Surgery in Geriatrics and Frailty: Vol. 2 No. 1 (2025)
- Dimitrios Damaskos, Carlo Vallicelli, Frailty in emergency general surgery and the role of the perioperative physician/geriatrician , Surgery in Geriatrics and Frailty: Vol. 1 No. 1 (2024)
- Martin Verheij, Andrew G. Robertson, Emergency laparoscopy in an ever-increasing geriatric population , Surgery in Geriatrics and Frailty: Vol. 2 No. 1 (2025)
- Hammaad Khalid, Abbey Boyle, Marina Yiasemidou, An audit evaluating quality and completeness of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) form documentation at Bradford Royal Infirmary , Surgery in Geriatrics and Frailty: Vol. 1 No. 1 (2024)
- Mauro Turrin, Stefania Simioni, Eugenia Bertin, Debora Tormen, Simona Frezzini, Gianfranco Mora, Invasive breast tumors in elderly women over ninety: a case series from a breast surgery center , Surgery in Geriatrics and Frailty: Vol. 1 No. 1 (2024)
You may also start an advanced similarity search for this article.
